This is an updated version of a medical student lecture I gave at National Guard Health Affairs in Riyadh.
To be continued

This is an updated version of a medical student lecture I gave at National Guard Health Affairs in Riyadh.
To be continued
I am a strong believer in performing both AHG and enzyme panels together in routine antibody workups. I especially feel this is important when the patient is R1R1 since I always want to rule out anti-c. Sometimes, anti-c is only identified in the enzyme phase.
This is a case from my files of an R1R1 patient with the following results:
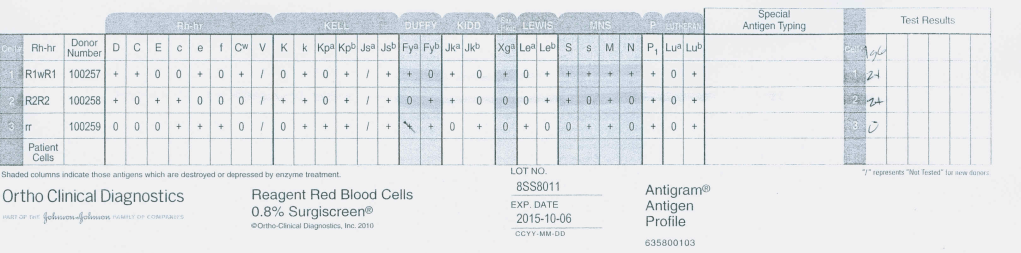
Antibody Screen:
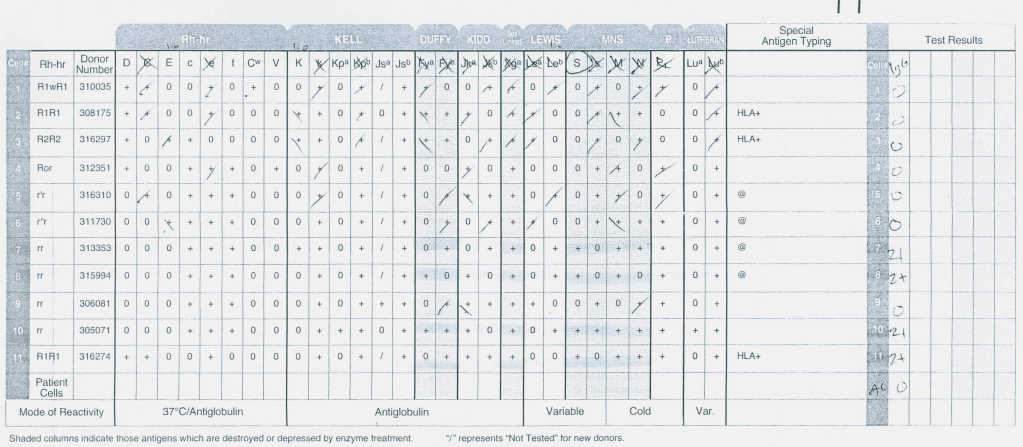
AHG Panel:
Enzyme Panel (Ficin):
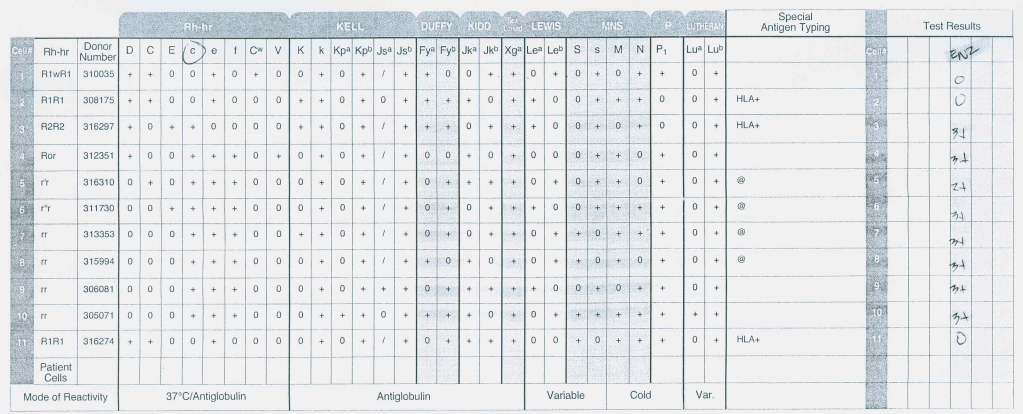
This anti-S is enzyme-labile but anti-c is revealed, only reacting at enzyme phase. The patient was Kell-negative so I selected S-negative, R1R1 K-negative RBCs for transfusion. Anti-c can be a dangerous antibody causing severe hemolytic disease of the fetus/newborn and sever hemolytic transfusion reaction. If only the AHG panel had been performed, the anti-c would have been missed.
Nowadays, if we have a multiply transfused patient with a complex antibody pattern, we might resort to RBC genotyping to help us resolve the antibody issues. Fortunately, there is one situation where we can quickly phenotype the patient by using hypotonic saline to lyse the transfused RBCs since the sickle cells are resistant.
The results can be quite clean and easy to interpret as in the following example using 0.4% saline:
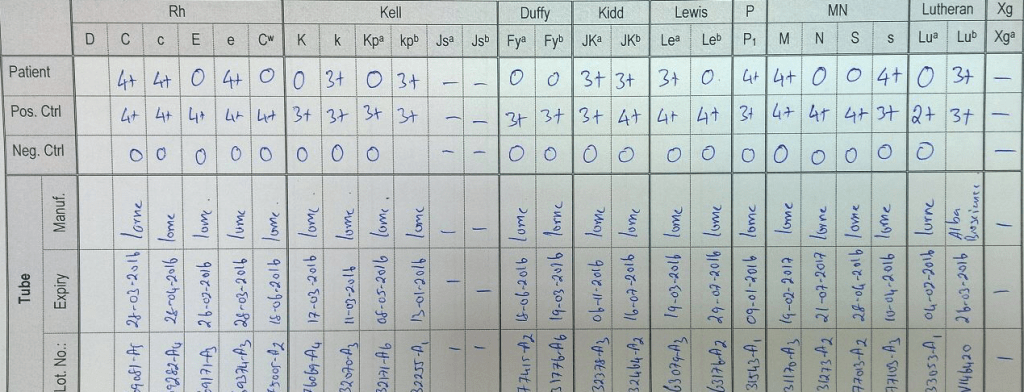
It is a lot cheaper to make dilute saline than an RBC genotype—and much quicker!
This was a teaching document for medical students and residents I made for NGHA Riyadh. I have updated it for leukodepleted components and platelet additive solution.
Immediate Steps for All Reactions:
After Transfusion is Terminated (except mild allergic, see below):
| Reaction Type | Signs and Symptoms | Etiology | Clinical Action |
| Allergic (mild) | Pruritus, urticaria (hives) | Antibodies to plasma proteins | Steps 1-3 above; administer antihistamines (PO, IM, or IV); resume transfusion if improved; if no improvement in 30 minutes treat as below. |
| Allergic (moderate to severe) | Hives, dyspnea, abdominal pain, hypotension, nausea, anaphylaxis | Antibodies to plasma proteins, including IgA (patient has anti-IgA antibodies) | Steps 1-5 above; administer antihistamines, epinephrine, vasopressors, and corticosteroids as needed; avoid future reactions by premedication and consider use of washed red cells if refractory. |
| Febrile (mild to moderate) | Fever, chills, rigors, anxiety, mild dyspnea | Antibodies to leukocyte antigens, (mostly HLA): cytokines | Steps 1-5 above; mild—administer antipyretics as needed; avoid future reactions by premedication and use of leukodepleted red cells and platelets |
| Acute lung injury | Fever, chills, dyspnea, respiratory failure | Antibodies form donor plasma to recipient WBCs; less commonly recipient antibodies to donor WBCs | Supportive therapy for respiratory failure, oxygen, mechanical ventilation, leukodepleted blood components, consider use of solvent detergent plasma, minimize plasma transfusions (use platelets in additive solution and leukodepleted RBCs in additive solution). |
| Acute hemolytic | Anxiety, chest pain, flank pain, dyspnea, chills, fever, shock, unexplained bleeding, hemoglobinemia/ hemoglobinuria, cardiac arrest | Hemolytic transfusion reaction; usually due to ABO incompatibility | Steps 1-5 above; treat shock with vasopressors, IV fluids, corticosteroids as needed; maintain airway; increase renal blood flow (IV fluids; furosemide); maintain a brisk diuresis; monitor renal status for acute renal failure. Monitor coagulation status for DIC; administer blood components as needed after etiology is clear. |
| Septic / toxic | Chills, fever, hypotension | Bacteria in contaminated blood | Steps 1-5 above; treat shock with vasopressors, IV fluids, culture patient and blood bag,antibiotics. |
5.2.1 PROCESS: DONOR QUESTIONNAIRE
Process:
References:
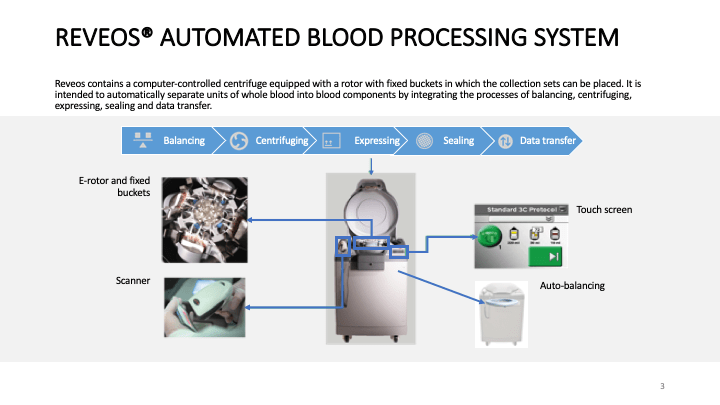
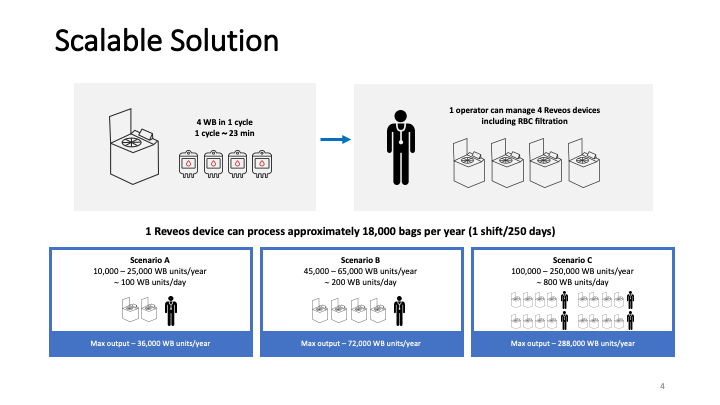
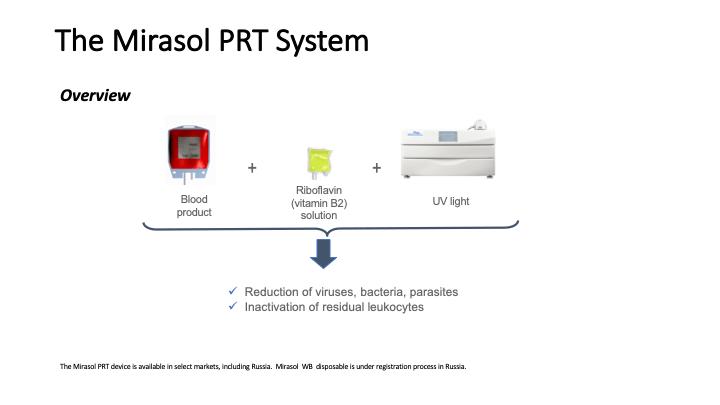
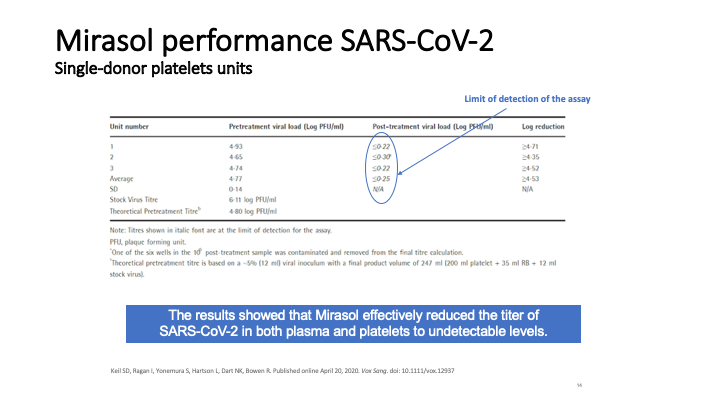
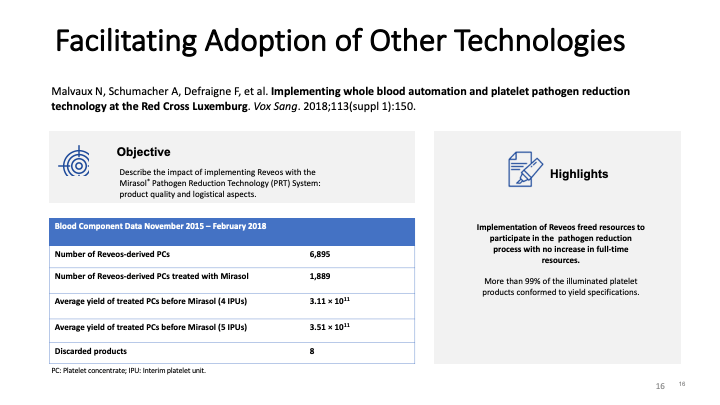
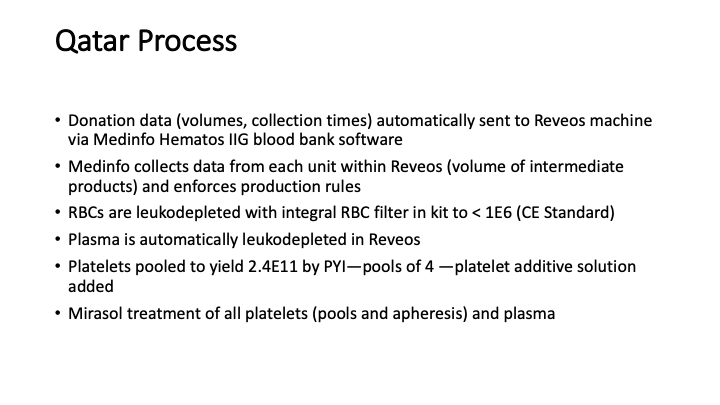
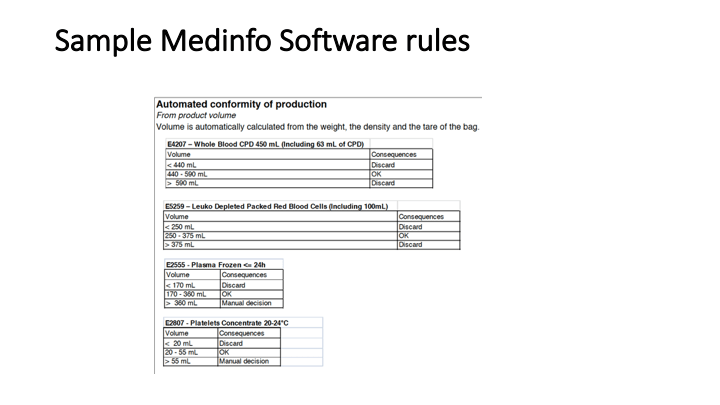
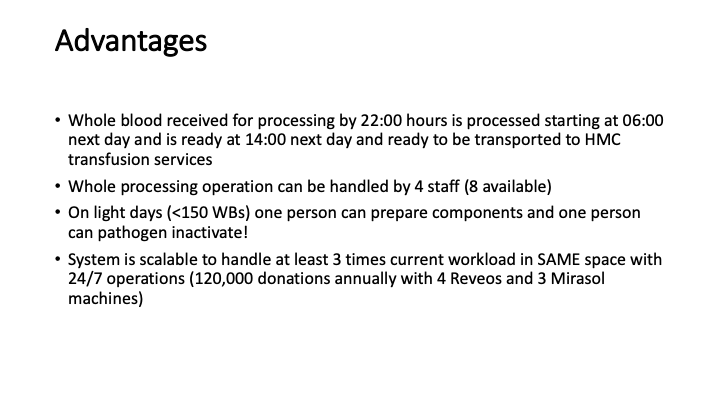
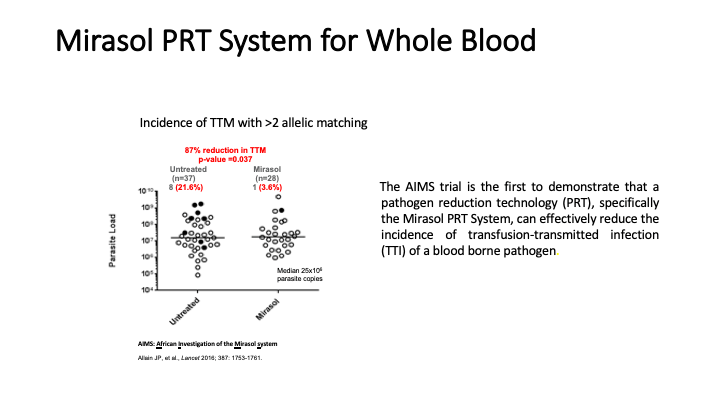
This is the virtual talk I gave at the Russian Transfusion Congress in Moscow on 13 May. It gives a brief description of automated component processing and riboflavin-based pathogen inactivation and then discusses the use of these technologies together to free up labor and enhance the quality of products, i.e. improved GMP, especially if a dedicated blood bank computer system is used to enforce production rules.

Policy Donor Medical Questionnaire
5.2 POLICY: DONOR MEDICAL QUESTIONNAIRE
Policy:
References:
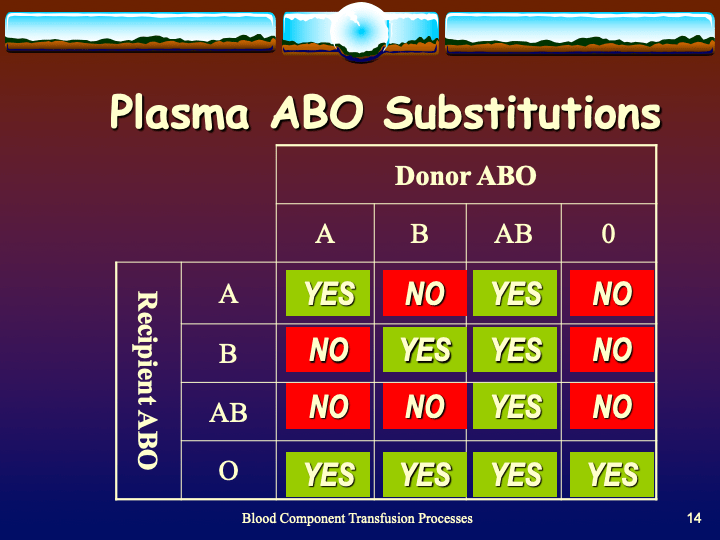
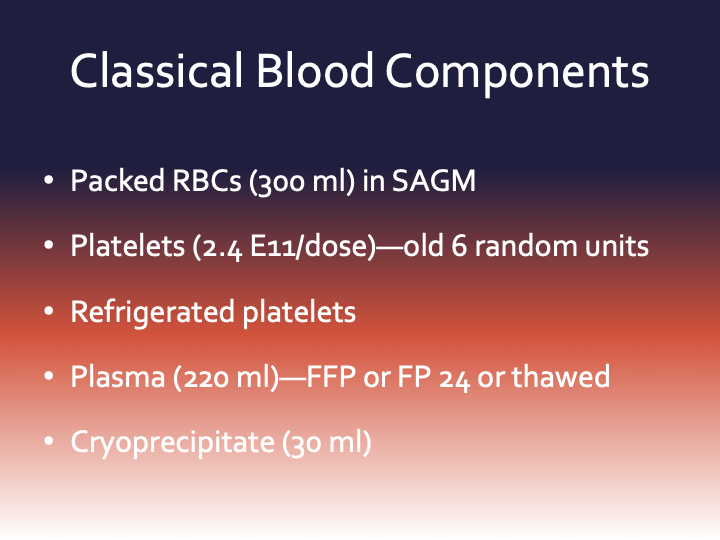
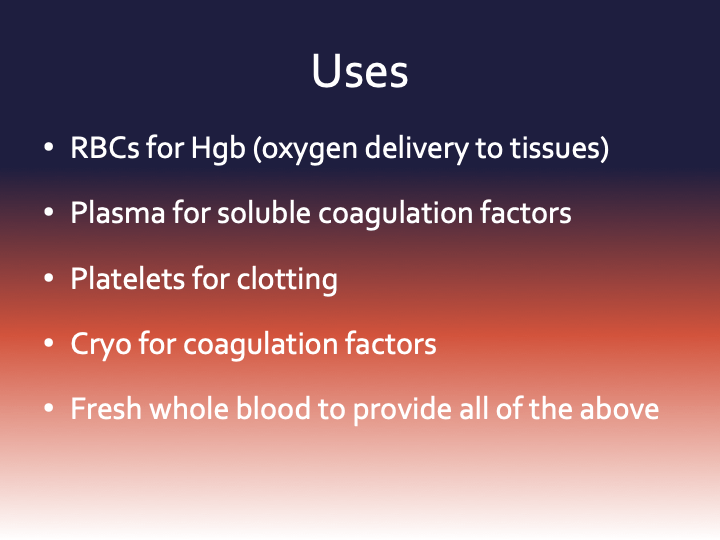
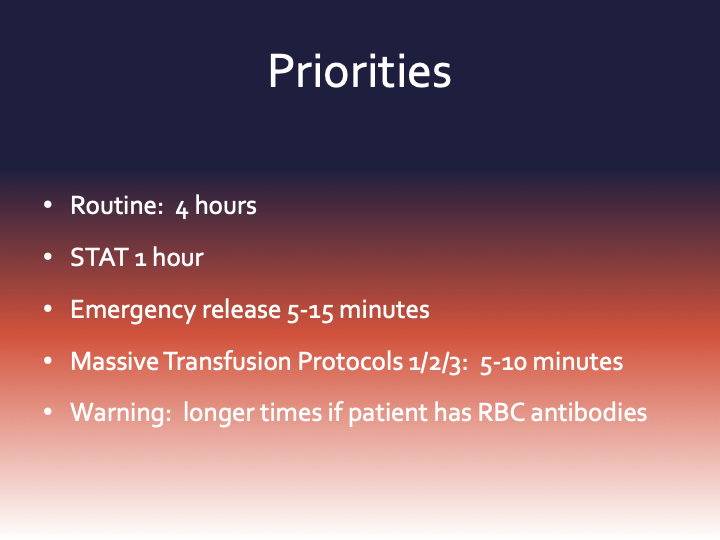
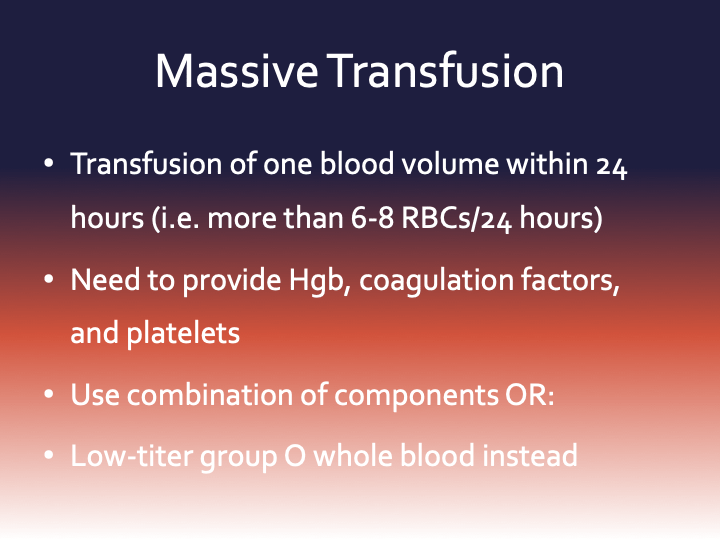
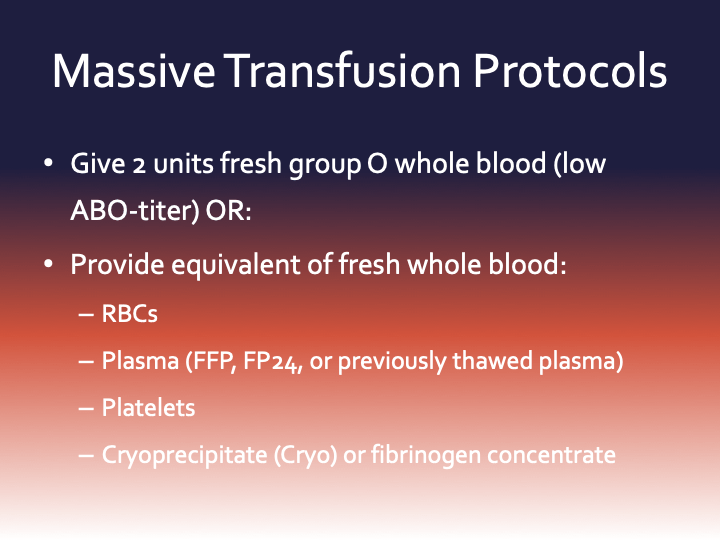
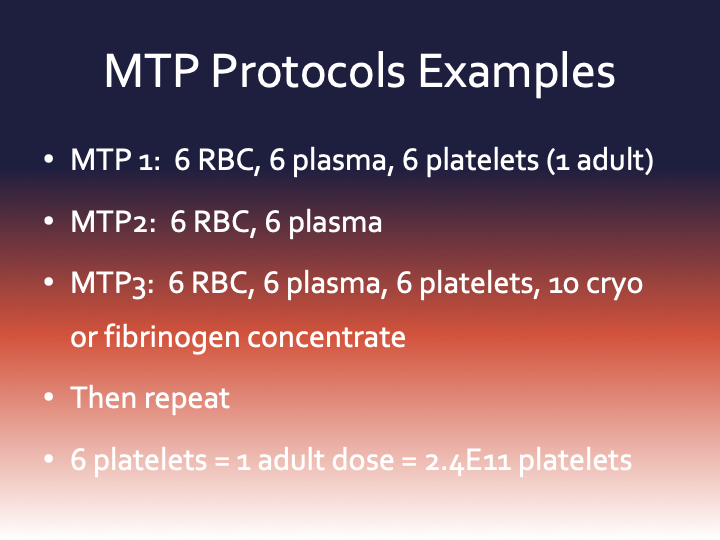
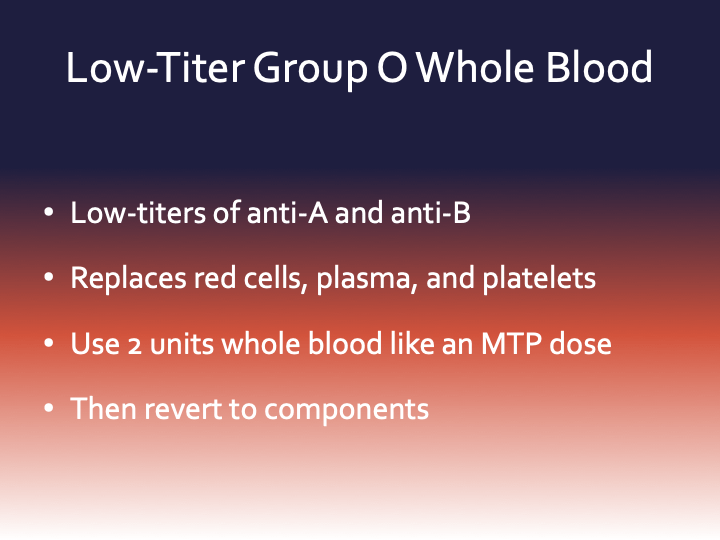
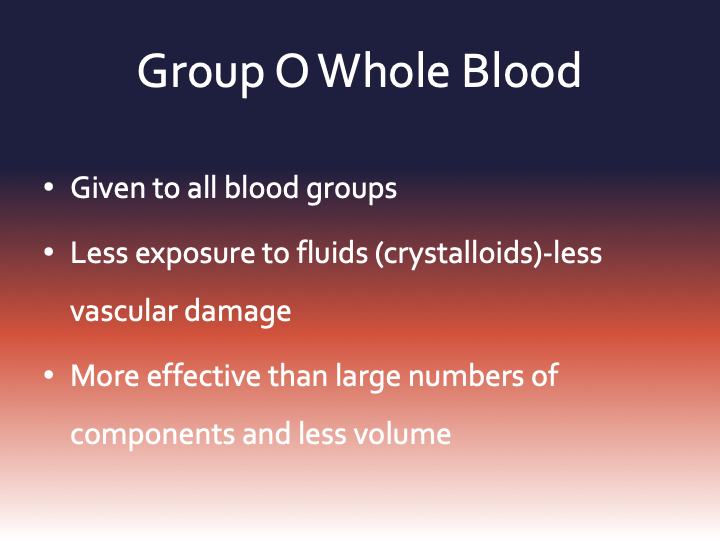
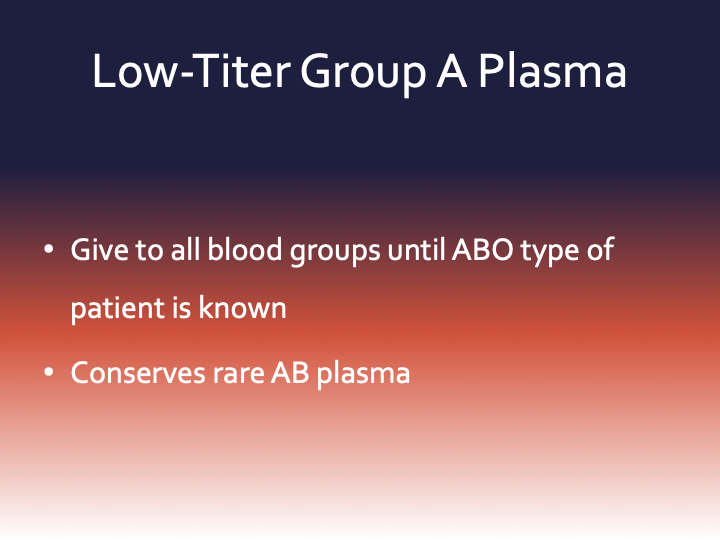
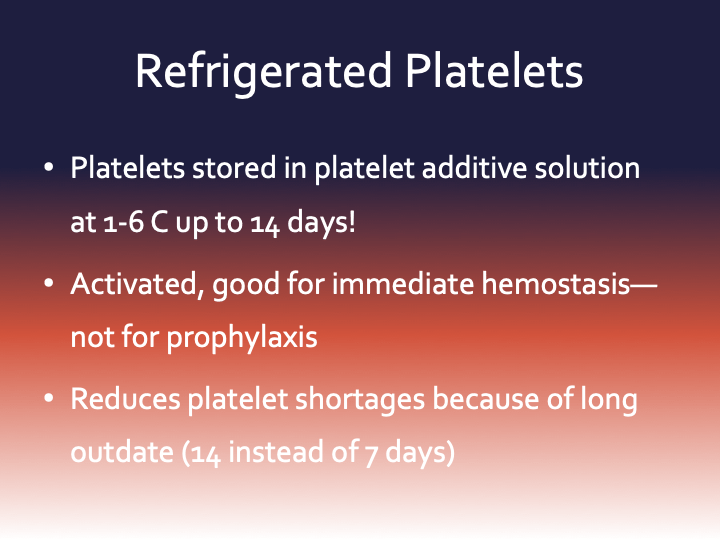
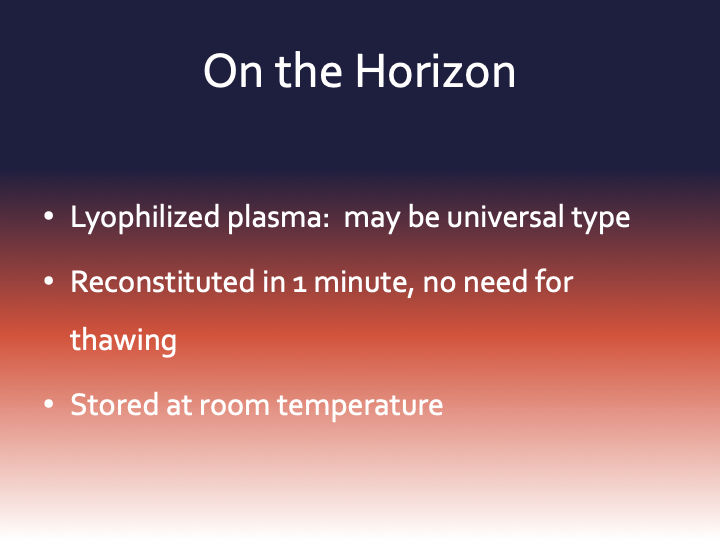
This is an updated version of a lecture I gave to medical students at National Guard Health Affairs in Riyadh. I have included new blood component types such as universal low-titer group O whole blood, universal low-titer group A plasma, and refrigerated platelets.
Super-Users: Engaging Laboratory Staff in Computer Operations
This is an update of a previous post.
It is critical to engage the technical, medical , and (blood bank) nursing staff in this process, That is why it is so important to identify a core of computer-literate users to help with the building and testing/validation.
I don’t mean finding staff who can already program or code. Rather, I mean staff that are astute with knowing their work processes and who had good skills with Microsoft Office and Windows or equivalent. I did not expect them to understand database structure or use structured query language. They were chosen for their ability to learn quickly and their meticulousness.
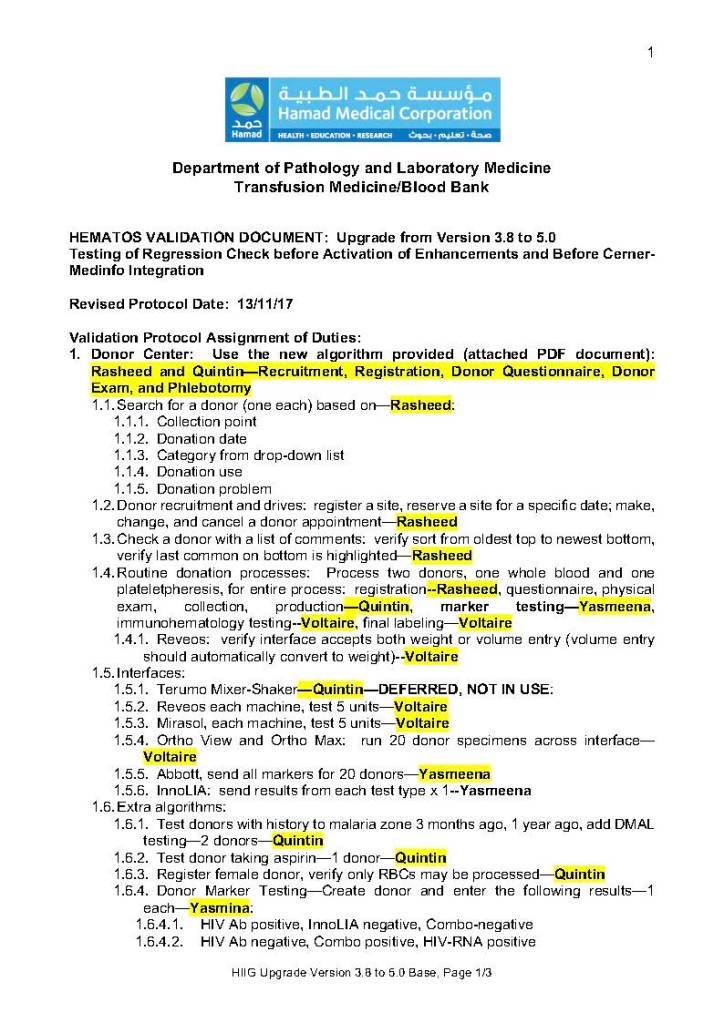
For our blood bank system, I chose computer-literate technical staff to be involved in the build from the very beginning. They learned how to test each module and to some degree support it. These became my Super-Users and to this day support the system for many tasks. These staff served as the system administrators and worked directly with me as the Division Head for Laboratory Information Systems. They were not full-time and still had their other clinical/technical duties. They liaised with the software vendors engineers.
Our blood bank system was NOT a turnkey system. It was custom designed according to our workflows. There were NO default settings!! We had to be remember, ‘Be careful what you ask for, you might get it!’ In some countries, approved systems are turnkey and may allow only few changes to the core structure and thus may not be this optimized for the needed workflow; often only cosmetic changes are permitted.
When we built our first dedicated blood bank computer system, the company would take a module and completely map out the current processes collaboratively with me. After this, I analyzed the critical control points and started to map out the improved computer processes that would take over. After that we would build that those processes in the software and test it. If it failed, we would correct it and test again…and again if necessary. Fortunately, the blood bank vendor did not charge us when we made mistakes.
Sadly, another vendor (non-blood bank), only gave limited opportunities to make settings. If wrong, there might be additional charges to make corrections. This other vendor really pushed the client to accept the default settings regardless whether or not they actually fit. End-users were selected to make and approve the settings, but they were only minimally trained on how to make the settings. It was a journey of the end-users being led to the slaughter—and being blamed for their settings when they accepted the vendor’s recommendations—they usually selected the defaults. There wasn’t enough time for trial and error and correction.
The blood bank system Super Users were an important part of our process. They were an integral part of the implement team and could propose workflows, changes, etc.—subject to my approval. They learned the system from the start and developed invaluable skills that allowed them to support the system after the build. Also, they could serve to validate the system according to the protocols I prepared. Moreover, I took responsibilities for their activities and they were not left out to hang.
Every hospital blood bank location and the blood donor center had Super-Users. These included:
The cost of using these staff? They were paid overtime and were relieved of other duties when working on Super User duties. This was much cheaper than hiring outside consultants who may or may not know our system well enough to perform these tasks.
By having a Super User at each site, I in effect had an immediate local contact person for troubleshooting problems who could work with the technical/nursing staff. We did not rely on the corporate IT department for support and worked directly with the software vendor. Response time was excellent this way.
The following document is a sample document of the assigned Super User duties during a validation.
5.1.1 PROCESS: Donor Registration
Process:
References: