It is easy to regurgitate data, but the key to using it successfully is to organize to maximize pattern recognition. Once a transfusion reaction has been called, the transfusion blood bank staff must expeditiously (STAT) perform testing to rule out acute hemolysis—one of the four fatal transfusion reactions (others being anaphylaxis, septic shock, TRALI/TACO).
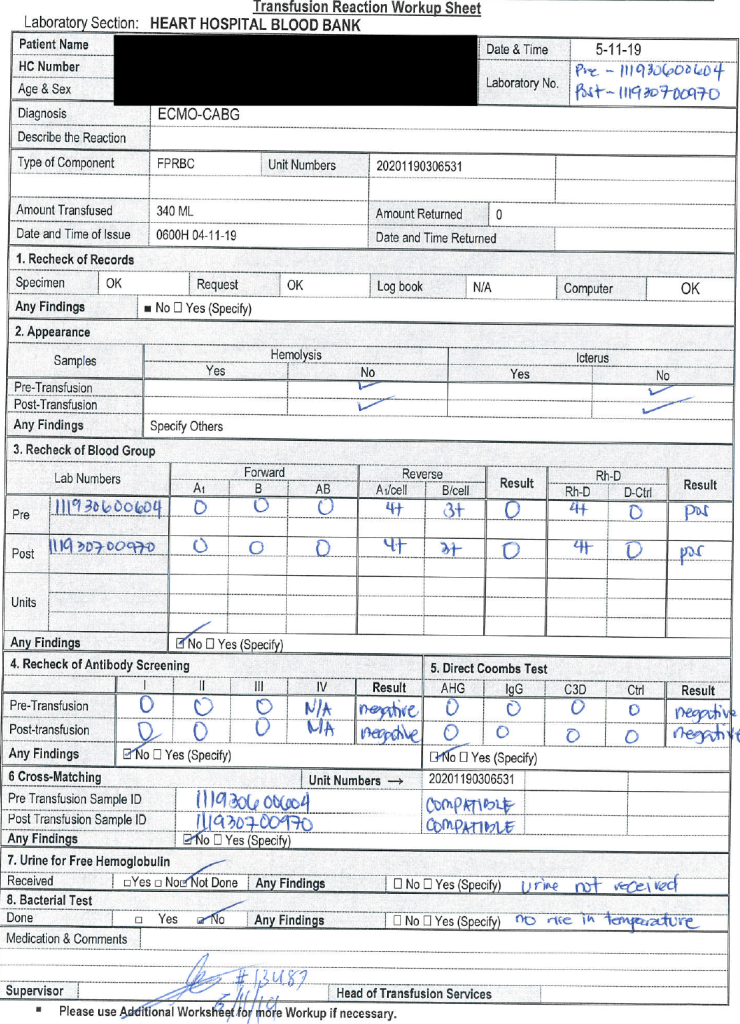
The attached form was designed by my staff and me based on my experiences at several institutions. It organizes the workup and helps ensure that all the testing and checks are performed. The clinical area calling the reaction will provide a transfusion form that includes the vital signs (pre-, post-, and during the transfusion) as well as the symptoms.
With these forms, life-threatening hemolysis can be ruled out and further studies made to rule out other serious adverse reactions.
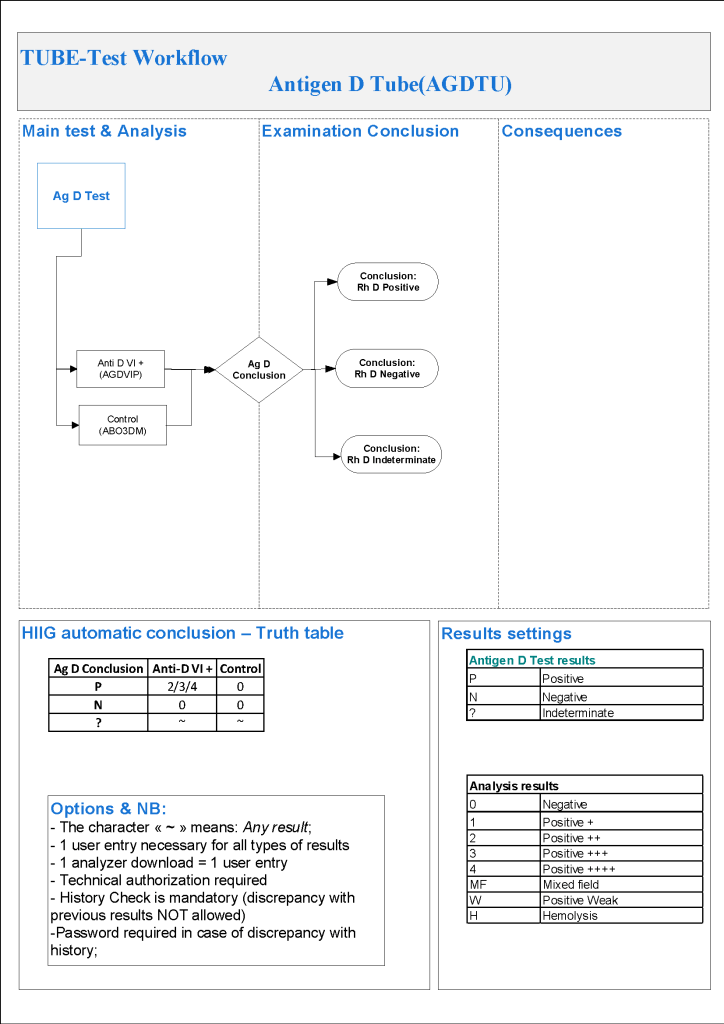
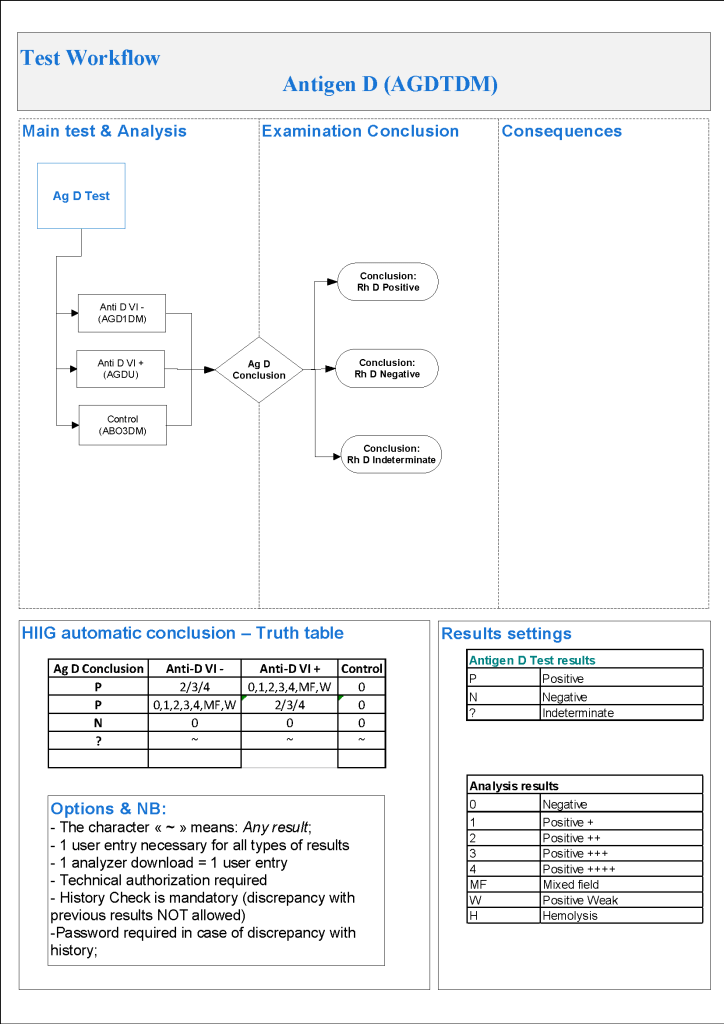
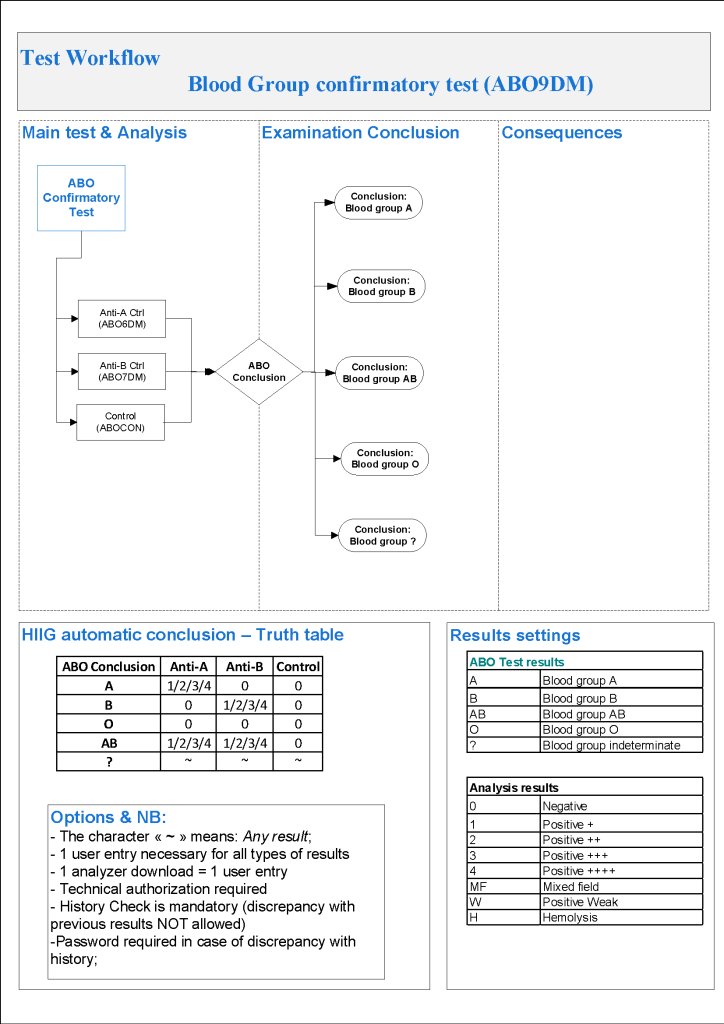
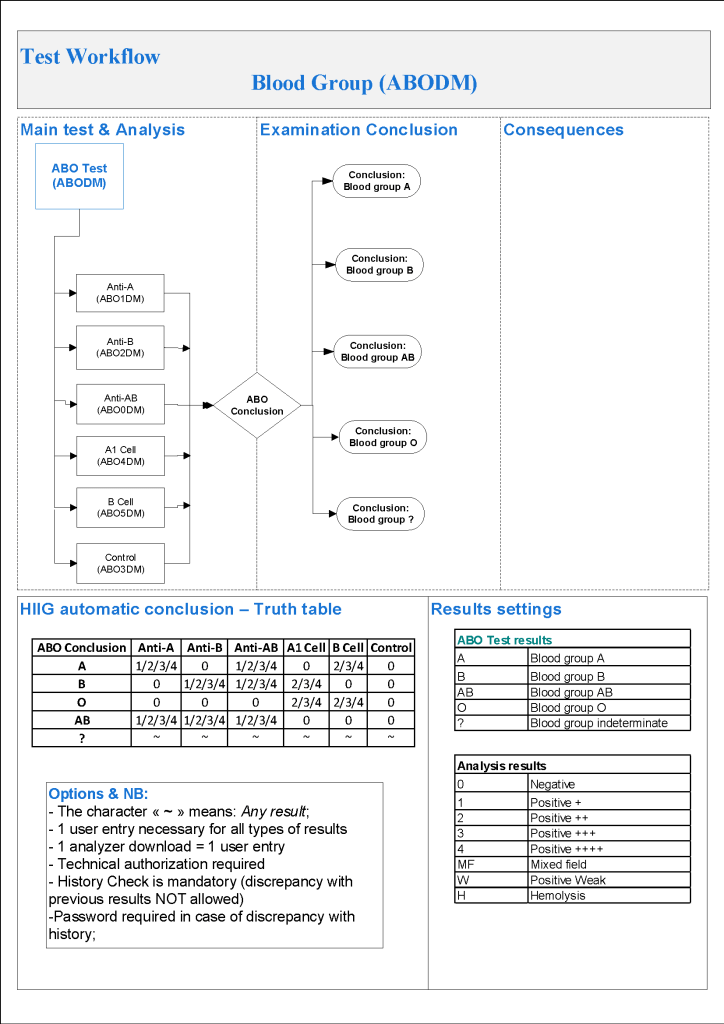
The data on this worksheet are entered into the Medinfo Hematos IIG Patient Module. The transfusion physician reviewing the workup will enter the type of reaction and recommendations. This will document the transfusion reaction for accreditation purposes.
10/10/20