Transfusion Medicine TM:
- Head, TMS, or the covering TM physician discusses case with the most responsible physician MRP; the plan of action mutually is agreed upon.
- Head, TM, or the covering TM physician gives verbal or written orders to apheresis nurse, including:
- Type of procedure (RBC exchange, plasmapheresis, plasmapheresis with column absorption, leukapheresis, thrombopheresis, stem cell collection)
- Machine parameters if indicated (e.g. fraction of cells remaining FCR, target hematocrit, unit hematocrit for RBC exchanges)
- Amount of exchange in liters (e.g. one-volume, two volume, etc.)
- Fluid balance (e.g. isovolemic, volume-reduced, volume enhanced)
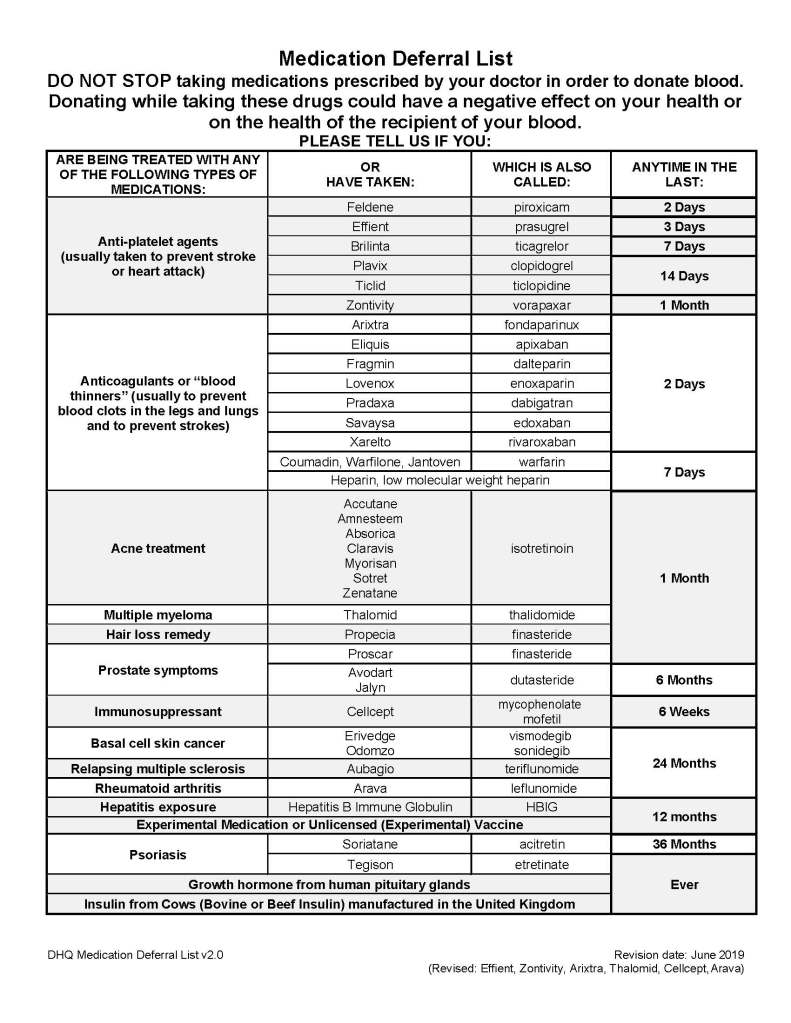
- Replacement fluids and volume (e.g. normal saline, 5% albumin, ACD-A, blood components, solvent-detergent treated plasma SDP)
- Calcium replacement (calcium gluconate IV)
- Orders for laboratory testing prior to and after the apheresis (usually CBC, PT, APTT, fibrinogen, total protein, albumin, calcium, LDH for TTP/HUS)
- Apheresis nurse convey the order to the ward/clinic.
- The requesting clinical service will place the order in the hospital information system.
- If a verbal order is made, TMS physician will sign his verbal orders, a copy of which will kept in the Apheresis Unit.
- If the hospital computer system is used, the TM physician will enter his orders and the apheresis nurses will take off the orders electronically.
- If a stem cell product is collected:
- TM will label it with a unique alphanumeric identifier barcode, i.e. an ISBT specimen label with check-digit that is generated by the Medinfo Hematos IIG system .
- Cellular Therapy Laboratory staff in conjunction with the apheresis nurse will sign-out the collection from TM to CTL using two donor identifiers: patient name and the unique alphanumeric sequence barcode (same as process of sign-out of blood component).
- Note: Use of Medinfo HIIG for stem cell collection is out of scope of TM.
Cellular Therapy Laboratory:
- Directly receive collected product from apheresis nurses will use the procedure outlined in 7.2 above.
Most Responsible Physician:
- Initiates request for apheresis with Division Head. Transfusion Medicine or covering Transfusion Medicine physician.
- Obtains informed consent from patient
- Arranges for proper venous access (rigid-bore central line or AV shunt)
- Is responsible for clinical support during the procedure
- Provides medication changes (e.g., substitution of non-ACE-inhibitors for hypertension therapy) as requested by the Head, TMS or Transfusion Medicine Physician
Ward/Clinic Nursing Responsibilities:
- Ward/clinic nursing staff effect written orders to obtain replacement fluids (albumin, blood components, crystalloid), calcium, and order tests in hospital computer.
- Ward nurses provide support (e.g., obtain medications, blood components, and miscellaneous items such as gauze, etc. and bring them to patient’s room) DURING THE PROCEDURE.
- As per Apheresis Policy (TRM-PM-410-000-000-01), the assigned staff nurse from the unit shall contact the Blood Donation Center.
- The assigned clinical staff nurse from the unit should call the local Blood Bank to request preparation of the requested components, e.g. RBCs, FFP, or cryoprecipitate and follow up.
- To avoid unnecessary delays before calling the Blood Donor Center Apheresis Staff Nurse the assigned unit staff nurse shall inform the Blood Donation Center Charge Nurse when the following have been completed and are available on the ward:
- Signed, informed consent
- A central line with a large bore double lumen.
- Completed blood laboratory results
- Only results within 24 hours of the intended procedure may be used to write the order.
- In some cases, more recent results may be required (e.g. TTP) at the discretion of the Transfusion Medicine physician.
- The ordered replacement fluids such as normal saline, thawed or liquid plasma, cryo-poor plasma, albumin and red cell units available in the ward
- Calcium gluconate (ordered amount in 100 ml normal saline) available
- The assigned apheresis nurse shall then perform the required therapeutic apheresis procedure strictly following the related TRM standard operating procedure.
Note:
- Apheresis is a SCHEDULED, high-priority procedure like other invasive procedures. The ward must make certain that the patient is available for the procedure at the scheduled time and place.
- Normally, apheresis procedures are performed 0600 to 1500 hours daily.
- The service is ONLY available 24/7 for emergency procedures outside this time frame. Emergencies must be approved by the TM physician.
- Transfusion Medicine does not guarantee that non-emergency procedures will be performed outside the 0600-1500 time frame.
- The most-responsible physician MRP is responsible for the patient’s concern form, establishing the proper venous access (rigid-bore central line), and providing coverage ON-SITE during the procedure. The apheresis nurse may not leave the patient’s bedside during the procedure.
- The apheresis nurse reports directly to the Division Head, Transfusion Medicine or the covering TM physician, not to the ward or MRP. Any issues about changing the apheresis orders must be approved by the Head, TM or the covering TM physician.
- All other procedures must be cancelled during apheresis.
- If the patient is not available at the specified, scheduled time, the procedure will be cancelled.
- If ward or MRP support is not available, the procedure will be cancelled.